
Acne
22 June 2022

Acne vuglaris is a very common skin problem that affects both males and females of all ages. Studies show that about 80% of teenagers and adults in their 30’s suffer from acne1-4. Acneiform lesions or pimples can appear on the face, neck, chest and back. Most of us would have encountered acne or pimples of some extent in our lives4,5. Some of us might have persistant, stubborn acne or pimples and deep scars from these pimples.
There are several causes of acne and types of acne. Genetics, stress, diet, makeup, hormones and skin care products are some of the factors that trigger acne. With more of us wearing surgical or cloth face masks to combat the spread of Covid-19 infections, acne related to wearing face masks is also on the rise.

This guide to acne will share the essentials and up-to-date findings of acne including:
• Types of acne
• Causes of acne
• What is hormonal acne
• Why does premenstrual acne occur
• How is adult acne different from teenage acne?
• Diet and acne
• Skincare for acne
• Medications for acne
• Treatments for acne

Acne is a skin condition involving the pilosebaceous unit which becomes blocked by dirt, sebum and dead skin. The pilosebaceous unit is also referred to as the ‘oil gland’ or ‘face pore’.
The pilosebaceous unit is made up of three components: the sebaceous gland (i.e. oil gland); arrector pili muscle and a hair follicle. What we see as the pores on our faces are the openings of the pilosebaceous unit. Large pores are related to skin oiliness. You can read more about enlarged face pore and how to shrink large pores in How to Get Rid of Large Pores: Myths and Truths.

There are 4 changes in the skin that lead to the development of acne6. We will learn about what causes these changes later in this blogpost:
1. Sebaceous gland hyperplasia and seborrhea
2. Follicular hyperkeratinisation
3. Proliferation of Cutibacterium acnes (Propionibacterium Acnes)
4. Inflammation and immune response.
Simply put, the sebaceous gland produces more sebum (i.e. increased oiliness) and the skin cells become more ‘sticky’ and block up the pilosebaceous unit. Cutibacterium acnes bacteria grows (because it feeds on sebum). Growth of Cutibacterium acnes bacteria triggers inflammation and immune reactions.
However, before you dismiss sebum as a harmful nuisance, sebum actually has a natural protective role in our skin! It reduces transepidermal water loss and protects against damage from infections and toxins. In treating acne, the key is striking a balance in reducing acne while ensuring that skin does not suffer from side effects such as dryness or peeling.
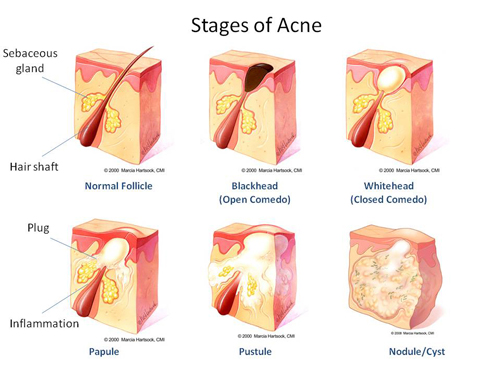
Most of you might be familiar with the red, pus filled swellings or pimples as acne. Did you know that ‘pre-acne’ lesions like blackheads and whiteheads are considered acne too?
Acne vulgaris is a spectrum consisting of: comedones (closed and open); papules; pustules and nodules. Here’s a breakdown on the different types of acne:

Comedones (clogged pores, blackheads and whiteheads)
When the pilosebaceous units (‘pores’) get blocked by dirt, dead skin, sebum, bacteria…etc, comedones (‘clogged pores’) form. Blackheads are open comedones; whiteheads are closed comedones.
Papules and pustules
When the comedones become inflammed and affect the dermis, the comedones form papules. Papules are the small, red and sometimes painful bumps classical of pimples.
If there is pus, the acne is called a pustule. Pustules look like papules, except that they contain yellow or white center. These are also the ‘juicy’ pimples that you may be tempted to squeeze. Don’t do that- you may end up with a scar.
Nodules and cysts (aka cystic acne or nodulocystic acne)
Nodulocystic acne is the most severe type of acne. This type of acne is painful, deeper and has a higher risk of scarring. Nodules and cysts have a higher risk of scarring as they run deeper in the skin.
acne treatment hinges on the correct diagnosis of acne morphology and treatment plan6. The outcomes and treatments differ depending on the type, severity, causes and complications of acne.
Open or closed comedones (i.e. non-inflammatory acne) are mostly cosmetic nuisances. On the other hand, papules; pustules; nodules and cysts (i.e. inflammatory acne) have a higher risk of complications. Post inflammatory hyperpigmentation (PIH); post inflammatory erythema (PIE); depressed acne scars and the distress need a doctor’s help8,9.
As you might have guessed, open and closed comedones can benefit from retinoids and treatments like chemical peels. Severe forms of acne like pustular acne and nodulocystic acne need antibiotics.

Hormones play a major role in acne vulgaris outbreaks. Hormones like androgens can alter the activity of sebaceous glands to cause more sebum to be produced i.e. hormonal acne10,11. Although there is no gene for acne, the predisposition of our sebaceous glands to these hormones is affected by our genes10,11.
Besides genetics, medications and use of occlusive wear (e.g. face masks) are major causes of acne10,11. Medical conditions (including hormone replacement therapy) that disrupt the balance of hormones in our bodies can also cause acne. Pregnancy alters the hormones in our bodies and are another cause of acne. Contraceptives, including intrauterine devices (IUDs) that contain hormones (e.g. Mirena) can also cause acne.
Stress, skincare and makeup and smoking are also possible factors10.
Related blogpost: Pregnancy Skincare Guide:
How to Avoid Acne From Wearing Face Masks
Pregancy Safe Skincare: What’s Safe and What to Avoid

The trigger for and worsening of acne is driven mainly by hormones, including teenage acne or puberty driven acne. When most of my patients in my clinic in Singapore talk about ‘hormonal acne’, they are referring to adult female acne related to their menstrual cycle.
Majority of women who suffer from adult female acne or ‘hormonal acne’ experience worsening of acne during the premenstrual period (i.e. before the period)12. Does this happen to you too? Do you notice more pimples and comedones about 1-2 weeks before your period? A smaller group of women notice that their acne flares during the menstrual or post menstrual period.
I’ll share more about hormones and acne in an upcoming post. This blogpost will focus on premenstrual female acne and the science of why it occurs.
The oiliness of our skin is affected by the hormones in our bodies. There are many hormones that affect the activity of the sebaceous glands. Androgens (sometimes referred to as the ‘male hormones’); estrogen; and progesterone play major roles in afffecting the sebum production by the glands. A shift in the balance can increase the sebum levels; which is one of the prerequisites for acne to occur.

In the menstrual cycle in females; the levels of hormones change in the first and second halves of the cycles. In the first half of the cycle, estrogen levels dominate. During the second half of the cycle, estrogen levels fall and progesterone levels rise. Finally, at the end of the second half the menstrual cycle, period occurs. The fluctuations in estrogen and progesterone levels is the cause of increased sebum and oiliness premenstrual period12,13.
Most studies show that adult female hormonal acne tends to occur in the lower face (jawline, around the mouth and sides of neck12,14. The reasons for this distribution is not clear12,14.
The type of acne in adult females is predominantly inflammatory pimples i.e. papules, pustules, nodules or cysts10. In adult female hormonal acne, the risk of complications like postinflammatory hyperpigmentation and scarring in 20% of sufferers15 .
This statistic is not surprising as adult female hormonal acne is mostly inflammatory; it is not merely blackheads or whiteheads. Medications will be needed to combat hormonal acne and prevent unsightly complications.

There is compelling evidence that our diet, specifically, high glycemic load diets worse acne16,17. High glycemic foods increase sebum levels, a risk factor for acne. The role of diet in acne is reviewed in detail in this blogpost Acne and Diet: Foods to Avoid for Less Pimples.
How high glycemic foods cause acne will be reviewed. The types of food that have also been linked to acne (e.g. dairy, fried food, supplements and probiotics also be covered).
Getting rid of acne vulgaris successfully depends on timely and appropriate treatment of acne and the causes of acne. Moving on next to how you can treat acne vulgaris (including adult female or hormonal acne) with skincare; medications and dermatological treatments.
The active ingredients and medical treatments for treating acne vulgaris focus on eliminating the steps in the pathogenesis of acne, namely4:
1. Reducing sebum production (i.e. oiliness)
2. Normalise keratinization (normalise clearance of skin cells)
3. Remove comedones and microcomedones
4. Resolving existing inflammatory lesions (i.e. papules, pustules, nodules and cysts)
5. Reduce colonisation of Cutibacterium acnes bacteria and inflammation
6. Prevention of comedones, papules, pustules, nodules and cysts

Please note that these examples do not substitute a medical consultation with a doctor. These over the counter active ingredients have the advantages of accessibility and less irritation than prescription grade topicals. However, they may not work for everyone as acne treatment is very personalised and complex.
Retinoids
Retinoids or vitamin A are the mainstay for treating acne of all types- including comedones, papules and pustules18. Vitamin A removes comedones, increases cell turnover and increases collagen formation in the dermis of the skin. This means that besides combating acne, retinoids lighten postinflammatory hyperpigmentation due to pimples.
There are different types of retinoids. Milder ones like retinols can be found in over the counter skincare. Stronger and more effective retinoids like retinoic acid (tretinoin) can only be obtained from a doctor in Singapore. To learn about the different types of retinoids; their differences, side effects and how to use them, my blogpost The Beginner’s Guide to Retinoids will share these details.
Benzoyl Peroxide
Benzoyl peroxide is another effective active ingredient for treating acne12. It targets several steps in the pathogenesis of acne including killing Cutibacterium acnes bacteria, reducing inflammation and removing comedones.
The main side effects of Benzoyl peroxide are skin irritation and bleaching of clothes.
Azelaic acid
Another effective anti-acne ingredient that kills Cutibacterium acnes bacteria and removes comedones19,20. You can read all about Azelaic acid in this blogpost Azelaic Acid: A Multi-tasking Skincare Active to Know. In Singapore, you can get Azelaic acid in skincare products but higher concentrations require a doctor’s prescription.

Acne pimple patches- do they work?
Discussing quick fix acne pimple patches by request from my patients. You’ve seen these before- small, transparent circle patches that claim to be pasted over ugly, offending zits. These pimple patches supposedly get rid of acne overnight. Two popular drugstore brands in Singapore are 3M’s Nexcare and CosRx are two very popular drugstore brands of pimple patches.
These pimple/ acne patches are in essence hydrocolloid stickers, which draw fluid out of the pimples. They also prevent you from picking at the pimple. Some pimple patches may also contain active ingredients like BHA/ salicylic acid and tea tree oil or even microneedles
Hydrocolloid dressing has been studied in the treatment of open wounds but there is only one study on hydrocolloid dressing in acne to date. This pilot study from Taiwan looked at the efficacy of 3M’s Acne Dressing on mild-moderate inflamed acne in 20 patients21. The results showed that in the 10 patients who received the hydrocolloid dressing had improved acne severity, redness and oiliness as compared to the 10 patients on control. The study also showed that the pimple batches also partially blocked out UVB rays, so the risk of post inflammatory hyperpigmentation may be reduced.

And that’s about it for the evidence on these hydrocolloid acne patches to date. There are no peer reviewed studies to lend credibility to overnight/ quick fix pimple patches. Pimple stickers/ acne patches have not been shown to be more effective than current methods of treating acne, so I remain a skeptic. Besides, pricking the skin with microneedles or microdarts and/or occluding them with ingredients can be irritating to the skin and carry a risk of infection.
Perhaps the only benefit of these acne stickers/ pimple patches may also stop patients from picking at their pimples. The newer generation of pimple stickers/ patches may be cute and colourful but they are not going to replace first line dermatological recommendations for acne for now, especially for cysts or nodules. If you have deep seated inflammation like cysts or nodules, you’ll need steroid injections to quickly reduce the inflammation.
Related blogpost:
Acne Steroid Injections & When Popping A Pimple Could Kill You
If you have inflammatory acne (i.e. papules, pustules, nodules and cysts) you should see a doctor soon to avoid complications like scarring. These types of acne and complications need a doctor’s help, not to mention medications and treatments. Skincare, facials, home based therapies will not help.
Even if you don’t have inflammatory acne, you will also benefit from seeing a doctor, especially if your acne is not improving. Prescription grade actives and medical treatments give faster results and kickstart your skin in the right direction for improvement.

Some examples of medications for treating acne are antibiotics, prescription grade retinoids (e.g. tretinoin and isotretinoin) and hormone treatments like contraceptives and spironolactone. The combination you need will depend on your acne. You can learn more about Isotretinoin in this blogpost, Is Isotretinoin (Roaccutane) Dangerous?
The treatment of acne is complex due to the highly variable nature of acne from person to person. Acne type, severity, causes and complications differ from person to person so acne treatments need to be personalised.
In my practice, topical treatments are the foundation for treating acne and maintenance to prevent recurrence of acne. I prescribe oral medications when required (e.g. inflammatory and severe acne) and discontinue oral medications as soon as possible.

In-clinic treatments for combating acne can also be combined with medications for faster results.
Q-switch laser
Q-switch laser is the mainstay laser for treating active acne vulgaris in Singapore. This laser reaches into the dermis to kill Cutibacterium acnes bacteria, reduce inflammation and decrease oiliness. Q-switch laser also lightens post-inflammatory hyperpigmentation (PIH) and brightens the skin.
My friend and beauty blogger, Pearlyn of Beautypeadia shared her experience with treating her hormonal acne and PIH with me in her blogpost, PIH, hormonal acne and pit scarring – my visit with Dr Rachel Ho. A picture speaks a thousand words so I’ll let her before and after photos and results in the blogpost do the talking.
Related blogpost
10 Things to Know Before Having Lasers for Your Pigmentation

Chemical Peels
Another workhorse for treating acne vulgaris in Singapore is with chemical peels. In general, chemical peels exfoliate the top layer of the skin to remove comedones, dirt, dead skin cells…etc. This allows younger and smoother skin to reach the surface.
In my clinic in Singapore, superficial chemical peels are the most popular chemical peel. Superficial chemical peels are very effective in removing acne and dirt on the outermost layer of the skin without penetrating the dermis. This allows for quick results with almost no recovery time.
Related post:
The Truth About Chemical Peels

LED Light Therapy
LED stands for Light Emitting Diode. In LED therapy, light is shone over the face to kill acne bacteria, reduce inflammation and decrease oiliness. A few studies show that LED therapy (blue light) helps to control acne. However, there are no large studies that demonstrate that LED therapy is more effective than existing acne treatments. You can read more about LED light therapy at home and in the clinic in LED Light Therapy Explained.
I use LED therapy to complement existing treatments for conditions like acne and for anti-aging in my clinic. I find that the Q-switched laser and chemical peels to be more effective than LED light alone for acne.
Acne begins with the blockage of the pilosebaceous unit; so clogged pores are the early manifestations of pimples. When these comedones become inflamed, larger pimples like papules, pustules, nodules and cysts can occur. Inflamed acne and long standing pimples have a higher risk of complications like dark spots (post inflammatory hyperpigmentation) and deep scars.
Hormones play a major role in acne outbreaks. Most of my patients experience hormonal acne or adult female acne that occurs before period. Diet, stress and inappropriate skincare have also been linked to acne vulgaris.
Getting acne treated correctly and early is key to good results. Besides using appropriate skincare, treatment of acne may also require medications and treatments. Acne treatment is complex and there are several factors that need to be taken in to the consideration. One of the common issues that patinets experience on their acne treatment journey is dryness, which can be managed with skincare. A
Thank you for having the patience to finish this post. Hope you found it useful. It was hard for me to include everything in because acne vulgaris is a large and complex topic. In upcoming posts, I’ll review the evidence for acne and diet and share how to treat acne complications (e.g. acne scarring and PIH).
1. Prevalence, morbidity, and cost of dermatological diseases. Kraning and Odland. J Invest Dermatol 1979;73(Suppl):395–401.
2. New understandings of the pathogen-esis of acne. Leyden. J Am Acad Dermatol 1995;32(5 Pt 3):S15–25.
3. Prevalence of facial acne vulgaris in late adolescence and in adults. Cunliffe and Gould. Br Med J 1979;1 (6171):1109–10.
4. Current concepts of the pathogenesis of acne: implications for drug treatment. Gollnick. Drugs 2003;63 (15):1579–96.
5. Recent findings in the epidemiologic evidence, classification, and subtypes of acne vulgaris. White. J Am Acad Dermatol 1998;39(2 Pt 3):S34.
6. Global alliance to improve outcomes in acne. Management Of acne: a report from a Global Alliance to ImproveOutcomes in Acne. Gollnick et al. J Am Acad Dermatol 2003;49(1 Suppl):S1–37
7. Management of Acne Vulgaris. Roman et al. (2016). JAMA, 316(13), 1402.
8. Persistent acne in women : implications for the patient and for therapy.Williams and Layton. Am J Clin Dermatol. 2006; 7(5):281-90. 9. Specificity of acne in women older than 25 years. Dumont-Wallon and Dréno. Presse Med. 2008 Apr; 37(4 Pt 1):585-91
10. Large-scale international study enhances understanding of an emerging acne population: adult females. Dréno et al. Global Alliance to Improve Outcomes in Acne. J Eur Acad Dermatol Venereol. 2015 Jun; 29(6):1096-106.
11. Acne Vulgaris.Sutaria et al. Stat Pearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020-.2019 Dec 13.
12. Adult female acne: a guide to clinical practice. Bagatin et al. An Bras Dermatol. 2019 Jan-Feb; 94(1): 62–75.
13. The effect of the menstrual cycle on acne. Stolla et al. Journal of the American Academy of Dermatology. 2001; 45(6), 957–960.
14. Adult-onset acne: prevalence, impact, and management challengesAdult-onset acne: prevalence, impact, and management challenges. Rocha and Bagatin. Clin Cosmet Investig Dermatol. 2018; 11: 59–69.
15. Postinflammatory hyperpigmentation: A comprehensive overview: Epidemiology, pathogenesis, clinical presentation, and noninvasive assessment technique. Silpa-Archa et al. J Am Acad Dermatol. 2017 Oct; 77(4):591-605.
16. Diet and acne. Bowe et al. J Am Acad Dermatol. 2010 Jul;63(1):124-41.
17. Significance of diet in treated and untreated acne vulgaris. Kucharska et al. Postepy Dermatol Alergol. 2016 Apr; 33(2): 81–86.
18. Expert committee recommendations for acne management. Zaenglein and Thiboutot. Pediatrics 2006;118(3):1188–99.
19. Multimodal Treatment of Acne, Acne Scars and Pigmentation. Shamban, and Narurkar. Dermatologic Clinics. 200; 27(4), 459–471.
20. Azelaic acid 20 % cream: effects on quality of life and disease severity in adult female acne patients.Kainz et al. J Dtsch Dermatol Ges. 2016 Dec; 14(12):1249-1259.
21. A pilot study on efficacy treatment of acne vulgaris using a new method: results of a randomized double-blind trial with Acne Dressing. Chao et al. J Cosmet Sci. 2006 Mar-Apr;57(2):95-105.